
Topic provided: Clinical & Diagnostic Labs ?
Clinical & Diagnostic Labs — Essential Instruments and Equipment
Summary: Modern clinical and diagnostic laboratories depend on a core set of instruments to ensure accurate, rapid and reliable results. This article describes the essential equipment categories, key selection criteria, and operational considerations.

Why proper equipment matters
Clinical and diagnostic labs directly impact patient care and public health. The right instruments — combined with validated methods, trained personnel and rigorous quality control — reduce diagnostic errors, shorten turnaround times, and support regulatory compliance.
Key equipment categories
Below are the essential instrument groups that most clinical and diagnostic labs should consider.
1. Molecular diagnostics and PCR systems
Thermocyclers, real-time PCR (qPCR) instruments and automated extraction systems are foundational for molecular tests (pathogen detection, genetic assays). Gradient-capable thermocyclers simplify assay development and optimization.


2. Detection systems and readers
Plate readers, luminometers, and chemiluminescence analyzers support ELISA, immunoassays, and many high-sensitivity tests. When choosing, prioritize sensitivity, dynamic range, and compatibility with common plate formats.
3. Containment and biosafety
Class II biological safety cabinets, appropriate personal protective equipment (PPE), and validated decontamination procedures are mandatory for handling infectious specimens. Regular certification and airflow testing are required for safety compliance.
4. Sterilization & waste management
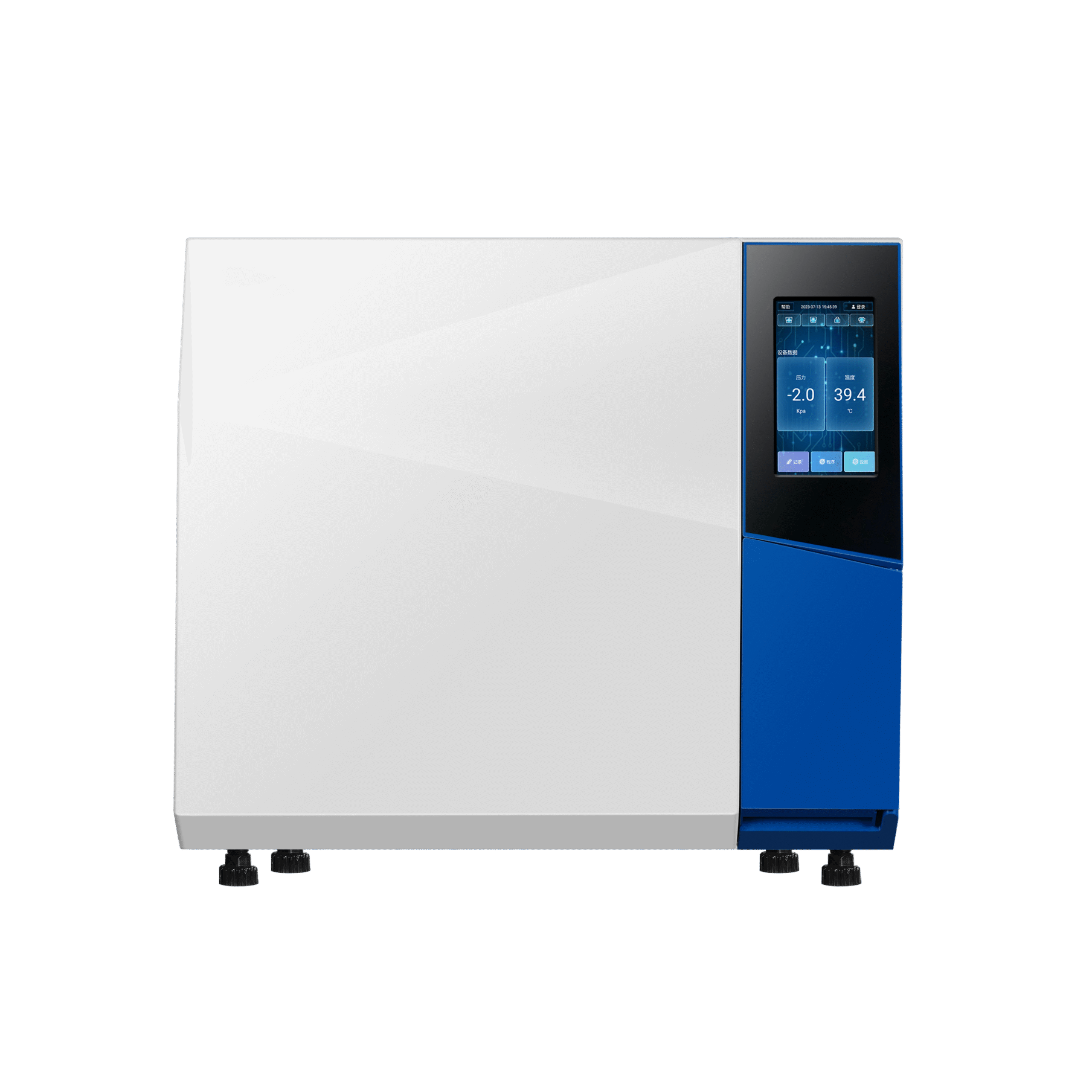
Autoclaves and validated chemical sterilants enable safe processing of contaminated materials. Waste segregation, documentation and proper autoclave validation protect staff and the environment.
5. Clinical chemistry, immunoassay and hematology analyzers
Automated analyzers increase throughput and consistency for routine blood chemistry, immunoassays and hematology panels. Important specs include throughput (tests/hour), sample handling automation, and LIS connectivity.
6. Centrifuges, incubators and microscopy
Refrigerated centrifuges, incubators and both brightfield and fluorescence microscopes are basic yet indispensable for sample preparation, culture work and morphological analyses.
7. Cold storage and sample integrity
Medical-grade refrigerators, -20°C freezers and -80°C ultralow freezers are needed for reagents and sample preservation. Look for alarms, data-logging and temperature mapping capabilities when procuring cold storage.
8. Precision liquid handling and consumables
Calibrated electronic pipettes, multichannel pipettes and high-quality filter tips, tubes and plates significantly improve assay reproducibility. Consumable quality often determines final assay performance.
9. Data systems and infrastructure
Laboratory Information Systems (LIS), middleware for instrument connectivity, secure backup, and UPS protection ensure data integrity and continuity of operations. Integration with hospital or clinic systems speeds reporting and reduces transcription errors.
Selection, maintenance and compliance
When buying instruments, evaluate service & support networks, consumable availability, total cost of ownership, and proven performance in clinical settings. Implement routine preventive maintenance, calibration schedules, and external quality assessment (EQA) participation to remain audit-ready (ISO 15189, CLIA where applicable).
Conclusion
A functional clinical & diagnostic laboratory requires a balanced mix of molecular instruments, detection systems, containment equipment, sterilization capacity, automated analyzers, stable cold storage and robust data systems. Prioritizing equipment quality, maintenance, staff training and regulatory compliance produces reliable diagnostics that clinicians and patients can trust.
